Magnetoencephalography (MEG) is a non-invasive diagnostic tool that can help neurologists and neurosurgeons evaluate and map brain activity before surgery. MEG offers a way to localize brain activity with a high spatial and temporal resolution, and represents a significant advance in the care of patients with brain tumors or severe epilepsy. A MEG scan is performed as an outpatient procedure — no overnight stay required. For some patients, MEG can replace invasive testing done in the ICU or in the operating room.
We are the first program in Wisconsin to offer MEG scans in a clinical (patient care) setting. In addition to clinical uses for neurosurgical planning, Froedtert & the Medical College conduct research studies using MEG to further develop this technology.
Mapping the Brain with MEG

MEG brings anatomical and physiological data together to yield images of brain physiology registered to the patient's brain structures.
MEG uses extremely sensitive and sophisticated sensors to record magnetic fields over the surface of the head. These fields are generated by the tiny electrical currents that flow between neurons (nerve cells) inside the brain. MEG scans these magnetic fields in the brain millisecond by millisecond. MEG is totally non-invasive.
Images are generated without the use of radioactive isotopes (used in nuclear medicine) or exposure to X-rays or external magnetic fields. MEG moves beyond existing technology in its ability to pinpoint in space and time normal and abnormal brain activity. By measuring the magnetic fields, the cell assemblies that produce each field can be located with an unprecedented millisecond temporal resolution.
For patients with brain tumors or for epilepsy patients who require surgery, MEG can help precisely identify the areas to be removed. This allows more complete and selective removal of the involved sections, while identifying brain tissue that must be spared to preserve important body functions. This more precise measurement also enhances the possibility of surgical success for patients whose tumor or epilepsy is considered inoperable.
Magnetic Source Imaging
After the MEG exam, the MEG recordings are combined with a magnetic resonance imaging (MRI) scan, which shows the actual structure of the brain. The combined scan, called magnetic source imaging or MSI, combines the structural image from an MRI and the time-resolved functional images provided by MEG. MSI is very helpful for showing areas of the brain that may be generating seizures or for locating a tumor, as well as for localizing areas of normal brain function with precise timing. MSI can provide neurosurgeons a detailed “map” that allows them to remove only damaged brain tissue while preserving healthy tissue.
Differences Between MEG and EEG
MEG measures magnetic fields, and EEG (electroencephalography) measures electrical potentials generated by the electrical activity of the brain. An important difference is that the skull and tissue surrounding the brain don’t affect the magnetic fields measured by MEG, while they strongly affect the electrical potentials measured by EEG.
When electrical signals from the brain pass through the skull and scalp, they are distorted and severely weakened. These same tissues, however, are transparent to the magnetic fields generated in the brain. Therefore, MEG offers a more accurate spatial estimate of brain activity than EEG. Compared to EEG, MEG allows for more usable and reliable localization of brain function. MEG can localize brain activity with a much higher spatial resolution than EEG, with the same millisecond scale time-resolution as EEG.
Make a MEG Appointment
For referring physicians: Please fill out our MEG order referral form. The completed form and any additional patient history can be faxed to Neurophysiology Desk at 414-259-1159 or be provided using HIPAA Compliant e-mails.
For patients: Your doctor will need to submit an order for a MEG study before we can schedule an appointment. Once we receive the form, we will contact you to schedule an appointment, subject to approval by your insurance plan.
If you have any questions about your appointment, please send an e-mail to the neurophysiology scheduler or call us at 414-805-2890.
Preparing for a MEG Scan
Magnetoencephalography (MEG) reveals which areas are involved in the control of a movement and how their activity is locked to the speed of the movement.
Because MEG detects the tiny magnetic fields from the brain, you will need to follow a few steps to ensure quality of the exam and optimal results:
- Remove all metal and jewelry before a MEG scan because these items will affect the quality of MEG recordings and subsequent analysis. Please tell your referring physician if you have metal medical or dental devices such as a pacemaker, patient-controlled analgesia (PCA) pump, vagus nerve stimulator, programmable ventriculoperitoneal shunt (VP) shunt, cochlear implant or braces. In addition, MEG technologists may need to evaluate certain implants (e.g., pins, clamps, clips, screws, coils shrapnel and cochlear implants) for metal content before the scan can be done.
- You will wear a hospital gown for the MEG scan. A locker will be provided to store all personal items.
- Women must wash their hair the day before the MEG scan. On the day of the scan, they must not use hairspray or wear makeup, which may contain traces of metal that can interfere with the scan.
- You must not have an MRI scan within one month prior to a MEG exam. An MRI can magnetize various body parts and alter the results of the test.
- If you have older dental fillings, we can demagnetize them before the MEG session with a degausser, a device that eliminates unwanted magnetic fields.
- Similar to other imaging procedures, it’s important to hold your head still during the recording of MEG data.
What to Expect During a MEG Scan
MEG recordings are done in special shielded room that blocks magnetic fields in the environment. This ensures that only the magnetic fields generated by the brain are detected by the MEG sensors.
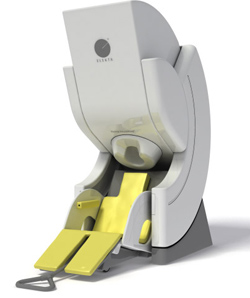
After entering the MEG room, you may either be asked to lie on a table bed or sit in a comfortable armchair. A special helmet containing the MEG sensors will be placed around your head. This special helmet will not cover your face, so you may even be able to watch a video and listen to music during the test. You will be asked not to move during the test, which runs for about one hour, with several short breaks. There is no loud noise during the test; the MEG environment is quiet and the recording is totally non-invasive.
To help identify the regions of the brain controlling movement and other important functions, various stimuli may be used during the MEG exam. These stimuli vary depending on the brain system that might be of interest to the your condition. For epilepsy, you may simply rest in the scanner and watch a movie or listen to music. For pre-surgical evaluation of brain tumors, the stimuli would focus on exploring the brain function as close as possible to the surgical target. This might concern language, memory, movements and various sensory systems (e.g., vision and touch). Stimuli may include sounds, a series of pictures, movies, tiny air puffs or very mild electrical stimulation.
Very often, an EEG recording will be done at the same time the MEG scan is performed.
If you have not had an MRI scan, which shows the brain’s structure, this will be done after the MEG session. This is needed so the MEG results can be combined with the MRI for a full picture and brain activations and structures. The combined scan — called magnetic source imaging — gives neurosurgeons a detailed “map” of damaged and healthy brain tissue to help plan surgery.
MEG Results
Trained MEG technologists ensure that MEG recordings provide the optimal quality of data. They work in coordination with the MEG physicists to provide in-depth analysis of the MEG recordings, possibly in conjunction with the anatomical information obtained from MRI. After several days, a detailed report is subsequently provided to your physician.