The Comprehensive Heart Failure and Transplant Program focuses on personalized care of advanced heart failure patients. We make sure our patients and their families understand all of their treatment options, which may include heart transplantation.
Medical Management for Heart Failure
Medical therapy is generally the first treatment approach for heart failure patients. Medications such as diuretics, beta blockers, angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) may be used to treat heart failure. Many patients may control heart failure symptoms well with medications for months, even years. However, if their symptoms worsen even with appropriate medications, other therapies may be considered.
Monitoring Heart Failure Symptoms After Diagnosis
New, implantable remote-monitoring technology, called CardioMEMS™, can help you manage your symptoms at home and allows your doctor to detect a decline in your condition even before symptoms occurs. Your cardiologist can adjust your medications and prevent a hospitalization.
Surgical Procedures to Correct Heart Failure
As heart failure progresses, surgical therapy may be necessary. The following procedures may be used to correct specific problems, stop further damage to the heart and improve the heart’s function.
- CardioMEMS™ Heart Failure System
- Coronary bypass surgery
- Mitral valve repair
- Ventricular remodeling (surgical ventricular restoration): An open-heart surgery performed to remove areas of dead heart tissue and reshape the left ventricle to help it work better. The procedure is usually done with coronary bypass surgery, with the aim of preventing the progression of heart failure.
- Cardiac resynchronization therapy (CRT) — Implanting a specialized biventricular pacemaker to re-coordinate the action of the right and left ventricles in patients with heart failure.
- Mechanical circulatory support devices, which can be used as a bridge-to-transplant or as destination therapy. These include:
- Total artificial heart (TAH) — A surgically implantable pump replaces the patient's damaged heart and performs the heart's function
- Ventricular assist device (VAD) — A mechanical support device is implanted to support the existing heart's function
- Heart transplant
Ventricular Assist Device (VAD)
Ventricular assist devices (VAD), which are surgically implanted mechanical pumps that help the heart pump blood, are being used with significant success. VADs can be a bridge to transplant – helping a patient survive months or years until a donor heart is available.
For patients who are not good transplant candidates however, the VAD can be the permanent therapy – also called “destination” therapy – improving their health and quality of life. Our success rate using a VAD as a bridge to transplant is significantly higher than the national average. Our program is also certified as a VAD Destination Therapy Program by The Joint Commission, an independent and nationally recognized health care certification organization.
Some advanced heart failure patients may not be good candidates for a heart transplant because of certain conditions such as severe lung, liver or kidney disease and cancer. For recent cancer patients, for example, the need to suppress the immune system after transplant to avoid rejection of the new heart could cause the cancer to come back.
If transplant is not an option, implanting a small, sophisticated VAD is a viable alternative as a destination therapy. Patients can return home and enjoy an improved quality of life with a VAD.
How Does a VAD Work?
A VAD is a mechanical pump that is surgically connected to the heart to help support blood flow and improve heart function. Different types of VADs are used, depending on the patient’s individual needs, and the power source is external, usually a mix of battery and electrical power.
A left ventricular assist device (LVAD) pumps blood to the aorta from the left ventricle. The HeartMate II® is one commonly used LVAD. A right ventricular assist device (RVAD) delivers blood to the pulmonary artery from the right ventricle or right atrium. A device that performs both functions is sometimes called a BiVAD.
VADs are most commonly implanted during an open-heart surgical procedure. Patients are usually connected to a heart-lung bypass machine during the procedure. A patient’s recovery experience depends on how healthy the patient was before surgery. VAD patients are also closely monitored before, during and after the procedure, and can return to many normal activities after they are released from the hospital.

The Froedtert & the Medical College of Wisconsin’s Heart and Vascular Center was awarded the Gold Seal of Approval by The Joint Commission for their Adult VAD Destination Therapy Program.
Barostim™ Baroreflex Activation Therapy
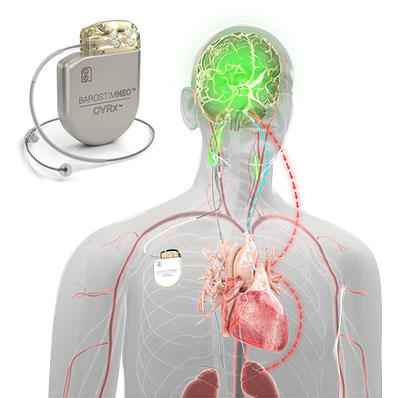
Barostim™ Baroreflex Activation Therapy is an FDA-approved heart failure therapy that uses neuromodulation to improve symptoms of heart failure in patients not eligible for cardiac resynchronization therapy (CRT). The Barostim device is implanted via a minimally invasive outpatient procedure that takes approximately 1 hour.
The implanted heart failure device does not touch the heart instead utilizes an electrode that lies on the patient's carotid artery. The electrical impulses sent from the neuromodulation device signal the brain to regulate the cardiovascular system. Barotsim has been shown to improve patient’s quality of life, exercise capacity and functional class, as well as a reduction in NT-proBNP levels (heart failure blood test).
CardioMEMS — Monitoring Your Heart at Home
CardioMEMS allows patients to measure pulmonary artery pressure (an early indication of worsening heart failure) at home. In a minimally invasive procedure, your cardiologist inserts a sensor in your pulmonary artery. Most patients go home the same day with a portable monitor and "smart pillow." Each morning, you will lay on the pillow to transmit your pressure readings to the advanced heart failure nurses at Froedtert Hospital.
If the pressures are out of your defined range, we typically adjust medications over the phone and watch your readings over the next several days. By catching pressure changes earlier, we hopefully can adjust your treatment before there is additional damage that could require a hospital stay. Most private insurance and Medicare plans cover the procedure and equipment, but we recommend you check with your insurance provider when considering the device.
Treatment for Edema or Congestive Heart Failure
Often, a person with heart failure may have a buildup of fluid in the tissues, called edema. Heart failure edema is called congestive heart failure (CHF). Traditional treatment for heart failure patients with edema has involved the use of diuretics (drugs that increase the excretion of water from the body). Over time, however, diuretics become ineffective, and continued use can cause more swelling.
Heart failure patients with edema (or other patients with other conditions that involve swelling in the legs and abdomen) may benefit from Aquapheresis™, a filtration system that removes fluid in patients for whom diuretics have stopped working. The system removes extra salt and water from the blood and body – up to 12 liters of excess fluid in 24 hours or up to 30 liters in 48 hours. Following the procedure, fluid loss is sustained for at least eight weeks.
The system connects to the patient’s bloodstream through catheters. Blood is run through a special filter and then returned through another vein. In addition to improving breathing and other symptoms, the process allows many patients to resume their cardiac exercise and rehabilitation programs as well as normal activities.
Virtual Visits Are Available
Safe and convenient virtual visits by video let you get the care you need via a mobile device, tablet or computer wherever you are. We'll assess your condition and develop a treatment plan right away. To schedule a virtual visit, call 414-777-7700.
Recognized as High Performing by U.S. News & World Report
Froedtert Hospital, Froedtert Menomonee Falls Hospital and Froedtert West Bend Hospital are recognized by U.S. News & World Report as high performing in heart failure care.More to Explore





