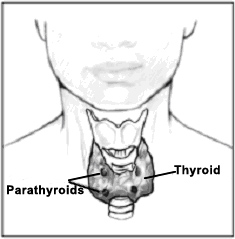
 The parathyroid glands are small, pea-sized glands located around the thyroid gland in the neck. The parathyroid glands regulate calcium balance in the body by secreting a hormone called parathyroid hormone (PTH).
The parathyroid glands are small, pea-sized glands located around the thyroid gland in the neck. The parathyroid glands regulate calcium balance in the body by secreting a hormone called parathyroid hormone (PTH).
Primary Hyperparathyroidism
Primary hyperparathyroidism is a hormonal problem that occurs when one or more of the parathyroid glands produce too much parathyroid hormone. The blood calcium becomes higher than normal, bones may lose calcium and kidney stones may form.
Primary hyperparathyroidism occurs in approximately 100,000 people each year, with a small percentage of cases occur in people with a family history of parathyroid disease. The most common cause of primary hyperparathyroidism is a noncancerous growth of the parathyroid gland.
Over time, patients with primary hyperparathyroidism are at risk for developing kidney stones, pancreatitis, gastroesophageal reflux disease, peptic ulcer disease, osteopenia, osteoporosis and bone fractures. The may also experience an overall feeling of fatigue, bone aches and pains, difficulty with memory and concentration, and mood swings. Patients with hyperparathyroidism may have severe symptoms, subtle symptoms, or none at all.
Multiple Endocrine Neoplasia (MEN) is a condition in which primary hyperparathyroidism is associated with tumors in other endocrine organs such as the pituitary and pancreas. MEN is a familial condition which involves genetic and hormonal abnormalities.
Hypercalcemia (high blood calcium) is a disorder that most commonly results from primary hyperparathyroidism. A variety of other conditions can cause elevated blood calcium. Laboratory evaluation (blood and urine) by the endocrinologist will help determine the cause of elevated blood calcium.
Diagnosis
Primary hyperparathyroidism is diagnosed by a combination of tests, including elevated calcium levels in the blood and elevated PTH levels. Other tests may be done to confirm the diagnosis or to assess complications of hyperparathyroidism. These include vitamin D levels, a 24-hour urine collection, and a measurement of bone density.
Surgical Treatment
Surgery is the only cure for hyperparathyroidism; there are currently no medications to treat primary hyperparathyroidism. When treated by experienced endocrine surgeons, the cure rate for primary hyperparathyroidism after surgery is greater than 95 percent.
Surgery is recommended for patients with kidney stones, bone fractures, or peptic ulcer disease. Surgery may also help decrease bone loss for patients with osteopenia or osteoporosis. Some patients also notice an improvement in their blood pressure, heart disease, energy levels and mood after surgery.
Minimally Invasive Parathyroidectomy
At the Froedtert & the Medical College of Wisconsin, our team of endocrine surgeons performs a minimally invasive parathyroidectomy whenever possible. This technique uses a protocol of preoperative localization studies and intraoperative parathyroid hormone monitoring. In select patients, this operation can also be done with sedation and local anesthesia. Many patients are discharged from the hospital on the same day of surgery.
Preoperative Localization
The goal of preoperative localization is to identify which of the four parathyroid glands is enlarged. At Froedtert & the Medical College of Wisconsin, this is done using a protocol of Sestamibi scanning, ultrasound and computed tomography (CT). This allows for a focused operation that minimizes the risk of complications from surgery.
Intraoperative Parathyroid Hormone Monitoring
The half-life of parathyroid hormone is only three to four minutes. During surgery, parathyroid hormone levels can be measured while the patient is still in the operating room. As a result, our surgeons are able to confirm that all overactive parathyroid tissue has been removed.
Recurrent Hyperparathyroidism
A small percentage of patients will develop recurrent hyperparathyroidism after surgery. The most common cause of recurrent disease is incomplete removal of all parathyroid disease at the initial surgery. In the hands of an experienced surgeon familiar with reoperative surgery, the success rate is greater than 90 percent with minimal complications.
Secondary Hyperparathyroidism
Secondary hyperparathyroidism is a problem in which the parathyroid hormone is elevated in response to kidney failure or to inadequate calcium or vitamin D (e.g., caused by vitamin D deficiency, intestinal or stomach surgery, or intestinal disease). In the absence of kidney failure, secondary hyperparathyroidism is often caused by vitamin D deficiency or stomach or intestinal disorders and is treated with calcium and vitamin D. Is this situation, surgery is not performed. Primary hyperparathyroidism is characterized by hypercalcemia (abnormally elevated calcium levels in the blood) and elevated PTH levels. It is the result of an abnormality of the parathyroid gland that disrupts the normal balance of calcium by producing too much PTH, even with high calcium levels.
Blogs, Patient Stories, Videos and Classes





