Although rare, soft tissue cancers (sarcomas) account for the majority of sarcomas, with about 9,500 new cases being diagnosed each year in the United States. Tumors occur in tissues that connect, support or surround other organs and structures within the body. These include muscles, tendons, nerves, blood vessels, fat and synovial tissues. A soft tissue cancer can appear as a lump (usually painless), but may also be present deep within tissues. Generally, there is no known cause, but occasionally lymphedema and prior treatment with radiation therapy can be contributing factors.
Types of Soft Tissue Sarcoma
There are numerous sub-types of soft tissue sarcoma:
- Fibrosarcoma and malignant fibrous histiocytoma occur in tissue that keeps muscles, bones and organs in place.
- Liposarcoma is present in fatty tissue.
- Leiomyosarcoma affects smooth muscle, as in the uterus.
- Rhabdomyosarcoma occurs in skeletal muscle.
- Epithelioid hemangioendothelioma, angiosarcoma, lymphangiosarcoma and Kaposi sarcoma are found in blood and lymph vessels.
- Synovial sarcoma (epithelioid sarcoma, clear cell sarcoma) are malignant tumors of unknown origin that commonly develop in the extremities.
- Malignant granular cell tumors and malignant peripheral nerve sheath tumors occur in peripheral nerves.
- Gastrointestinal stromal tumors (GIST) mostly develop from specialized cells within the gut.
- Desmoplastic small round cell tumors (DSRCT) often begin in the peritoneum, the tissue lining the abdominal cavity, and can spread from the peritoneum to other organs, most commonly the liver and lungs.
Diagnosing Soft Tissue Sarcoma
In addition to a patient's personal and family medical history and a physical exam, the physician may recommend one or more of the following diagnostic studies:
- X-rays: to image various areas of the body
- CT scans: cross-sectional images that can reveal if a tumor has spread
- MRI scans: use magnetic energy to produce detailed pictures inside the body without X-rays; can be especially useful in distinguishing connective tissue cancers from benign tumors
- PET scans: image the body's metabolic activity to show if cancer has spread
- Biopsy: the removal of small tissue samples or cells; the only certain way to make a diagnosis of cancer.
Treating Soft Tissue Sarcoma
Soft tissue sarcomas are usually treated with a combination of surgery, medical oncology, and radiation oncology. Surgery is typically the primary modality. Radiation oncology is often used to facilitate tumor removal and to decrease the risk of local recurrence. Chemotherapy administered by medical oncologists may play a role in treating or minimizing the risk of developing metastatic disease.
Surgery
Soft tissue sarcoma often affects a patient’s physical function and appearance. Surgery aims to remove the cancer, as well as restore physical function and esthetic appearance. When removing a soft tissue sarcoma, it is absolutely critical that a “cuff” of normal tissue is taken from around the tumor cells to minimize the risk of the tumor recurring at the local resection site. Our surgeons are specially trained to remove cancers and achieve safe "margins" in surgery. This helps assure that all of the cancer was removed to prevent recurrence.
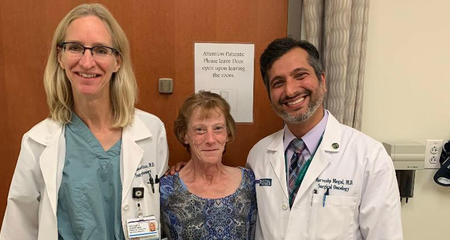
Our cancer surgeons and plastic surgeons work in tandem to achieve those goals. The unique procedures they have developed allow cancer surgeons to be aggressive in removing cancerous tissue to safe "margins," while ensuring a return to function and an esthetically-pleasing reconstruction.
Unlike other facilities that perform multiple surgeries on a patient, we have perfected the technique of completing cancer and reconstructive surgeries in a single operation, whenever possible. When the cancer team finishes, the reconstructive team begins its delicate task of rebuilding muscle volume, and replacing fat, nerve and skin.
We make every effort to streamline and optimize the care of patients with bone and soft tissue sarcomas. Patients scheduled for surgery are evaluated by our Preoperative Clinic team to ensure surgery is done as safely as possible and any peri-operative questions are answered completely. Following surgery, a team (including doctors, nurse practitioners, and physician assistants with specialized expertise in the medical management of the complex tumor patient) works hand-in-hand with the surgical team to optimize the care of this challenging and unique patient population.
Plastic Surgery
After a patient has had surgery to remove a sarcoma, plastic surgeons use specialized surgical techniques to replace tissue and close the surgical wound.
The goal of plastic surgery is to restore the most natural appearance and functioning of soft tissues (skin, fat, blood vessels and nerves). The plastic surgeon may use tissue from other areas of the body to provide natural coverage of exposed artificial joints, bones, blood vessels and nerves. The donor tissue may come from the abdomen, thigh or back. When possible, surgery to remove the cancer and reconstructive surgery are performed in a single operation.
Read more about plastic surgery’s important role in treating sarcomas.
Medical Oncology
Our Sarcoma Program team may also recommend chemotherapy to treat soft tissue cancer. Anti-cancer drugs may be administered before surgery, to shrink the tumor, or after surgery to minimize the risk of the cancer occurring elsewhere in the body. Froedtert & MCW medical oncologists administer single agents and combinations of drugs known to be effective on soft tissue cancers.
Radiation Oncology
Radiation treatment may be recommended to treat your soft tissue sarcoma.
A combination of conservative surgery and radiotherapy has been shown to achieve excellent local control in sarcoma patients following margin negative surgery. Radiotherapy can be given before or after surgery, providing equivalent local tumor control.
One advantage of pre-operative radiation is the delivery of a smaller radiation dose to a smaller target volume when compared with post-operative radiotherapy. This translates into fewer long-term treatment complications and better function of the extremity, as demonstrated in Phase III randomized clinical trials. Other potential advantages of giving radiotherapy before surgery include shrinking the tumor and reducing the risk of tumor cell seeding at the time of surgery.
The main concern around pre-operative radiotherapy is the risk of increasing the rate of delayed wound healing when compared with post-operative radiation.
However, surgical resection of your soft tissue sarcoma might be performed before you have radiation treatment. This is especially true when the histology diagnosis from the biopsied tissue (pathology report) is inconclusive or unknown, or when there is significant concern about wound healing.
Therefore, deciding whether radiation treatment before or after surgery is best for you should be determined after a discussion with a physician who specializes in soft tissue sarcomas.
Types of Radiation Therapy
Brachytherapy (internal radiation therapy) — Brachytherapy is a method for destroying cancer cells by placing a small radioactive source next to the tumor. When combined with surgery, it is a very effective way to treat soft tissue sarcomas. Brachytherapy allows physicians to deliver radiation to a tightly defined target area, while avoiding healthy tissue and critical structures.
There are two types of brachytherapy:
- Interstitial brachytherapy: This is often performed after surgery. Your physician inserts several tiny plastic catheters in and around the tumor. Through these catheters, low-dose-rate (LDR) or high-dose-rate (HDR) radioactive substances deliver a high dose of radiation to the tumor bed several days after surgery. Each dose exposure takes several seconds to minutes, and the radioactive substances are removed after each treatment session. The catheters are removed after the last treatment. The entire treatment series, including surgery, takes one to two weeks.
- High-dose-rate (HDR) brachytherapy: Recently, HDR brachytherapy has been increasingly used for sarcoma treatment. Radiation intensity can be altered using the CT-based HDR brachytherapy planning system. Therefore, radiation dose to the tumor cells in the tumor bed can be maximized, while radiation to nearby normal tissue structures can be minimized. In addition, HDR brachytherapy is available as inpatient or outpatient treatment.
External beam radiation therapy — In external beam radiation therapy, cancer cells are destroyed by radiation fields generated by a device outside the body. It can be effective at controlling cancer, and offers a good ability to limit side effects. External beam radiation may also be given in combination with brachytherapy and drug therapy.
External beam radiation therapy is used in several different scenarios. It is often given before or after surgery, or it may be indicated for patients who are not good candidates for surgery because of age or other health problems. External beam radiation can also help relieve the pain of bone metastases.
- Conformal radiation: A key goal in external beam therapy is producing radiation fields that conform tightly to the tumor target. “Conformal” radiation enables physicians to deliver a higher dose of radiation to cancer cells. The results are greater ability to destroy cancer while avoiding damage to adjacent normal tissue structures.
- Several technologies: We offer several different radiation systems for providing conformal radiation. One class of systems uses Intensity Modulated Radiation Therapy (IMRT), a technique for precisely delivering hundreds of thin radiation beams (rather than a few wide beams) to a tumor. A computer determines the best way to deliver treatment by “modulating” the intensity of each beam. The Clinical Cancer Center’s TomoTherapy® unit is an advanced IMRT system that combines precise 3-D imaging from an onboard CT scanner with highly targeted radiation fields.
Virtual Visits Are Available
Safe and convenient virtual visits by video let you get the care you need via a mobile device, tablet or computer wherever you are. We’ll gather your medical records for you and get our experts’ input so we can offer treatment options without an in-person visit. To schedule a virtual visit, call 1-866-680-0505.
More to Explore