A rare cancer is one that happens in fewer than 6 out of 100,000 people every year. As a group, rare cancers make up around 25% of all cancers.
Rare cancers aren’t rare to us. If you are newly diagnosed with a rare cancer or have an advanced cancer that has not responded to standard treatments, you can be confident in choosing our team of internationally recognized physicians.
Our Rare Cancer and Precision Medicine Clinic brings together a team of highly experienced specialists in rare tumors who have particular expertise in evaluating the molecular alterations associated with these tumors. The team works in tandem with doctors from the Cancer Network’s disease-specific programs when patients with rare or advanced cancers need more options. These specialists apply precision medicine therapies as appropriate, along with more traditional treatment approaches individualized to each patient.
We are also happy to provide second opinions. Getting a second opinion is appropriate when you want to find new treatment options, confirm a treatment plan is the right one or even mid-treatment to make sure you’re going down the right path. You may also seek a second opinion if standard treatments aren’t working to eliminate your cancer.
Why Are Rare Cancers Hard to Treat
Many factors make a rare cancer harder to treat.
- It can take a long time to diagnose.
- It’s hard to find a doctor who knows a lot about a particular rare cancer and how to treat it.
- Your oncologists may not agree on how to treat your cancer because they may not know a lot about it — they may not have treated a patient with it before.
- To find the right doctor to treat your rare cancer, you may have to travel far from home.
- Your doctor may not know who is an expert in your rare cancer that he or she can refer you to.
- There may be fewer or no FDA-approved drugs for a rare cancer and limited or no clinical trials for a rare cancer.
- There may be little available information, even in medical journals, about a specific rare cancer to generate ideas on how to treat it.
- Researchers may lack tumor tissue to further their research.
- If there is an idea of a drug or combination of drugs that might work for a rare cancer, it can be hard to find enough patients with the cancer to test the idea in a clinical trial.
Using Precision Medicine to Diagnose Rare Cancers
Genetic studies and large groups of data like the All of Us study, can point to an uncommon diagnosis — or may reveal your risk of developing other types of cancer. We carefully analyze tumors using molecular profiling (a type of genetic study) to produce an accurate diagnosis that informs the treatments that will be most effective for your specific cancer. We also use large data sets to help reveal patterns, relationships and other insights that can help guide treatment.
Cancers Treated in the Rare Cancer and Precision Medicine Clinic
Any patient with a rare/ultra-rare tumor or a tumor with an unusual molecular profile may be evaluated in our Rare Cancer and Precision Medicine Clinic. The team also sees patients who have advanced cancers that don’t respond to standard treatment, as well as patients with common cancers who need a specialized treatment strategy.
There are around 200 rare cancer types. The list below is but a small sample of the rare cancers we treat. It is by no means a comprehensive list; patients with many types of rare cancers are considered for treatment in our Rare Cancer and Precision Medicine Clinic. For many of these cancers, there are no FDA-approved treatments; however, using a precision medicine approach, our rare cancer experts create treatment plans using approved treatments in unique combinations for each individual. They also enroll patients in clinical trials that allow treatment individualization
-
Fibrolamellar Cancer
Fibrolamellar cancer, also called fibrolamellar carcinoma, is a cancer of the liver. Although most liver cancers happen when people have livers damaged by cirrhosis or infection with a virus, fibrolamellar cancer develops in people with healthy livers. Because this disease is extremely rare, data is scarce due to that factor. Researchers think fibrolamellar cancer makes up between 1% and 5% of liver cancers. Men and women get this cancer in equal ratios, and it is diagnosed more in young adults (median age 25).
-
Erdheim Chester Disease (ECD)
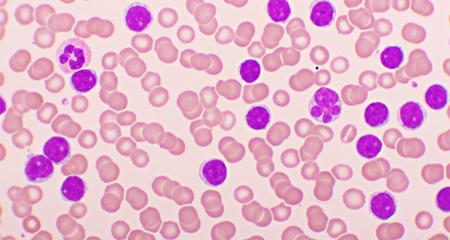
Erdheim Chester disease (ECD) is an ultra-rare type of blood cancer, with only about 100 cases reported in the medical literature. It often shows up in middle age, diagnosed when a person is in their mid-50s. Slightly more men develop ECD than women. There is no cure for ECD.
ECD affects different systems of the body, and its location in the body can vary from person to person. Multiple tissues and organs over-produce histiocytes (white blood cells), which are normal immune cells. Histiocytes have a role in fighting infection and injury by finding and destroying invasive microorganisms or cell debris. When they accumulate in larger than normal amounts, they most often affect the skull. However, ECD can also affect the spine and long bones. Tissues and organs that can be involved include the skin, lungs and other organs. Doctors sometimes find ECD in the pituitary gland.
-
Ameloblastoma
Ameloblastoma affects less than 1% of people in the world. Anyone can develop this disease but it is more typically seen in people ages 30 to 40. It is not common in in children younger than age 10.
Ameloblastoma is not usually cancerous, but rarely, it can become malignant, and very rarely, it will metastasize (spread) within the body to areas such as the neck and lung lymph nodes. About 80% of ameloblastoma cases are associated with mutations in two genes. It usually develops in the jaw within cells that make up the enamel lining of the teeth but can start in the gums. The most common type is aggressive and can grow large, extending into the jawbone.
-
Sarcomatoid Lung Cancer
Sarcomatoid lung cancer is a type of non-small cell lung cancer, making up just .1% to .4% of all lung cancers. It is seen more in men who are older and are heavy smokers. People are usually diagnosed in middle or advanced stages of the disease. It is an aggressive cancer and often spreads beyond the lungs.
-
Epithelioid Hemagioendothelioma (EHE)
Epithelioid hemagioendothelioma (EHE) starts in cells within the blood vessels. It is not hereditary. It can start anywhere in the body but often starts in the lungs, liver or bones. EHE happens in just one out of every 1 million people in the world. Incidence may be higher because the disease is very challenging to diagnose. The most common age range for this diagnosis is people between ages 30 and 50 but it can happen in children and people older than 50.
-
Castleman Disease
Castleman disease is diagnosed in between 4,000 and 5,000 people in the U.S. each year. Incidence is not limited by age, gender, race or ethnicity — it can happen to anyone. Because it is rare and tends to mimic other diseases, it is hard to diagnose. Castleman disease is made up of four main types, including unicentric and three types of multicentric Castleman disease. It is a disorder involving cells in the lymph nodes and shows up as enlarged lymph nodes (or a single enlarged node). The lymph system is part of the immune system, which normally fights cancer and other invaders.
With Castleman disease, cells that normally protect the body from disease become overactive. They produce inflammatory substances, and they do not return to their usual protective role. It must be diagnosed with a lymph node biopsy and sometimes, blood and imaging tests. Some people have only mild symptoms; others have severe symptoms and dysfunction in multiple organs.
-
Hepatoblastoma
Hepatoblastoma is a type of liver cancer. It is the most common pediatric liver cancer, usually developing in children younger than age 3. Hepatoblastoma is very rare in adults and carries a poor prognosis because it does not cause symptoms for a long time, and by the time symptoms appear, the tumor has grown very large.
-
PEComa
PEComa — perivascular epithelioid cell tumor — develops in the blood vessel walls and can grow in any part of the body. It can affect men and women at any age. It is so rare, that it is diagnosed in only one person in a million each year — globally. It is usually diagnosed incidentally (during diagnostics done for an unrelated reason). PEComa can be benign, or it can be an aggressive sarcoma that can metastasize.
-
Embryonal Sarcoma of the Liver
Embryonal sarcoma of the liver typically develops in the right lobe of the liver. This cancer is aggressive, with a propensity to spread. It is found mostly in children between age 5 and age 11, but can happen in adolescents, too. Very, very rarely, adults are diagnosed with this cancer, and only a small number (about 100) of adult cases are reported in medical literature. Symptoms can be non-specific, making diagnosis challenging; it is often a process of ruling out other diseases.
-
Merkel Cell Cancer
Merkel cell cancer is a type of skin cancer, affecting around 1,600 people each year in the U.S. The chance of developing it increases with age, and about three quarters of people diagnosed with Merkel cell cancer are older than age 65 when diagnosed. It affects men slightly more than women.
Merkel cells are found in the top layer of the skin. Cancer can form if Merkel cells grow erratically. Other names for Merkel cell cancer are Merkel cell carcinoma, neuroendocrine carcinoma of the skin and trabecular cancer. Most commonly, Merkel cell cancer starts in skin that gets more sun exposure. It starts as a single, painless lump that is red or violet, firm and dome-shaped or raised. It is aggressive and tends to grow and metastasize (spread) quickly. It is the second most common cause of skin cancer death behind melanoma. When Merkel cell carcinoma metastasizes, its first targets are typically nearby lymph nodes followed by spread to other lymph nodes, skin in distant body areas, the brain, the lungs, other organs or bones.
-
Hyalinizing Clear Cell Carcinoma
Hyalinizing clear cell carcinoma is a tumor that starts in the salivary glands. It makes up less than 1% of salivary gland tumors, and only a small number of cases are reported in medical literature. It usually presents in people ages 60 and older but can affect a wide variety of ages. Most often, it starts as a painless lump. Hyalinizing clear cell carcinoma can be challenging to diagnose because it can be confused with a benign growth. When found in early stages, it has a good prognosis with appropriate treatment but can metastasize and recur after treatment.
-
Metastatic Basal Cell Cancer
While basal cell carcinoma is a common skin cancer — making up about 80% of skin cancers that are not melanoma — metastatic basal cell carcinoma is extremely rare. Incidence varies from .0028% to .55%. It is diagnosed most often in middle-aged men.
-
Neuroblastoma
Neuroblastoma (adult) can develop in nerve cells in any part of the body — typically occurring in immature cell forms such as in embryos or in fetal cells. It is considered rare in children — and incidence is even lower in adults, affecting about 1 in 10 million each year. When diagnosed in adults, it is aggressive and is typically located in abdominal and pelvic areas, as well as the thoracic spinal cord, olfactory region and mediastinum (part of the chest that holds the heart) and olfactory region — the part of the nose that allows a person to detect different scents.
Neuroblastoma is a cancer of the sympathetic nervous system, which is made up of cells that communicate with the body by putting out tiny amounts of hormones. Neuroblastomas can be asymptomatic (no symptoms) or they can release hormones that result in a wide range of symptoms, including many that can look like common conditions.
-
Mucinous Adenocarcinoma
Mucinous adenocarcinoma develops in cells that produce mucus, and these tumors secrete a large amount of mucus. It makes up only about 1% of cancer diagnoses. It develops most commonly in the colorectal tract and any organs that have many glands such as the stomach, breast, ovaries and lungs. Symptoms depend on the area of the body affected, and some people have no symptoms until the cancer is advanced.
-
Chordoma
Chordoma is a cancer that grows from tissue inside the spine. When diagnosed, it is often found at the base of the skull or near the tailbone. However, it can occur anywhere along the spine. Chordoma is diagnosed in just one in a million people in the world each year. Depending on where the tumor is located, it can cause pain in the legs or bladder or bowel incontinence (tumors near the tailbone), or it can cause headaches or double vision (skull base tumors).
-
Malignant Giant Cell Tumors
Giant cell tumors represent 5% to 6% of primary bone tumors (tumors that start in the bones). These tumors are usually benign but rarely, they can become cancerous. Malignant giant cell tumors are essentially a type of sarcoma. These tumors can be primary, usually arising from benign giant cell tumors, or secondary, diagnosed after treatment, including radiation therapy. How many people develop malignant giant cell sarcoma (incidence) remains a question, as these tumors are challenging to diagnose or are misdiagnosed as benign.
Benign and malignant giant cell tumors look similar during exams with conventional forms of imaging tests. Biopsies can miss malignant tumors that exist with benign tumors if the biopsied samples are not extensive enough. Testing for gene mutations to help differentiate benign vs. malignant giant cell tumors is being evaluated.
-
Paraganglioma
Paraganglioma is a neuroendocrine tumor that grows outside the adrenal gland near blood vessels and nerves. Only about two of every 1 million people get paraganglioma – usually when they are between 30 and 50 years old. Paragangliomas can be hereditary or they may be connected with changes in certain genes. While the disease can be without symptoms, some people can have a fast heartbeat, headaches, high blood pressure, excessive sweating and tremors. Diagnostics include blood and urine tests to check for hormone levels, as well as imaging tests to find the tumor’s location and size and to figure out if it has metastasized (spread) to other parts of the body. Around 35% to 50% of paragangliomas will metastasize.
-
Adenoid Cystic Carcinoma
Adenoid cystic carcinoma can develop in children, but it is usually diagnosed in adults between the ages of 40 and 60, skewing more toward females (about 60%). It affects about 1,200 people in the U.S. per year. Adenoid cystic carcinoma typically starts in the salivary glands but can happen in other places in the head and neck. It can also develop in areas such as the prostate gland, the skin, the cervix and the breast. Symptoms vary, depending on the part of the body in which the cancer begins. While the cause is not confirmed, researchers think this disease could be related to genetic changes.
Adenoid cystic carcinoma grows slowly but it can move into nerve fiber sheaths and lymph nodes near the area where the cancer started. Adenoid cystic carcinoma can spread or metastasize, with about half of cases spreading to the lungs.
-
Phyllodes Tumors
Phyllodes tumors are typically benign growths (around 60 – 75%) in the breast. However, they can be malignant, which happens in less than 1% of all breast cancer cases. Phyllodes tumors are most often seen in women between the ages of 35 and 55 but can happen to women of any age. They are different from more common types of breast cancer, because they develop in the connective tissues of the breast instead of in breast ducts or glands. They are considered a type of sarcoma and can grow quickly or suddenly.
To optimally treat rare cancers, our treatment approach encompasses all aspects of cancer care, including standard therapies like surgery, radiation therapy and chemotherapy. We also emphasize precision medicine treatments including immunotherapy and gene-directed, targeted therapies based on the unique molecular signature of your tumor.
Experts in Rare Cancer
Our rare cancer experts include world-renowned specialists who are highly respected in their fields not only for advancing developments in precision medicine but also for their leadership in designing clinical trial programs and research in genomics and genomic testing. They may offer the greatest opportunity for successful treatment because they know about and are able to provide options not widely available. Options may include unique combinations of medications for your cancer and clinical trials from the largest cancer clinical trials treatment program in the state.
We are a high-volume cancer treatment network with specialists who are experienced with diagnosing and treating rare and advanced cancers. You benefit from the input of not just one doctor, but from a multidisciplinary team of experts from all relevant specialties. They meet in disease-specific cancer conferences and collaborate to determine the most effective approach to treating your cancer. As an academic medical center, our investments in cancer research, clinical trials and precision medicine are helping accelerate treatment breakthroughs for rare and advanced cancers — so we can deliver the right care when you need it most.
Rare Cancer and Precision Medicine Experts
Recognized as High Performing by U.S. News & World Report
Froedtert Hospital is recognized by U.S. News & World Report as high performing in three adult specialties and 16 procedures and conditions, including cancer.
Blogs, Patient Stories, Videos And Classes