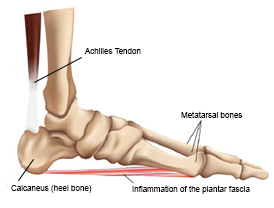
 Plantar fasciitis is the most common cause of pain on the bottom of the heel. It refers to inflammation of the plantar fascia, a thick, fibrous band of tissue that begins on the bottom part of the heel, and attaches on the metatarsal heads (ball of the foot), helping to form the arch of the foot. The inflammation suggests degeneration in the plantar fascia, and is rarely due to acute trauma.
Plantar fasciitis is the most common cause of pain on the bottom of the heel. It refers to inflammation of the plantar fascia, a thick, fibrous band of tissue that begins on the bottom part of the heel, and attaches on the metatarsal heads (ball of the foot), helping to form the arch of the foot. The inflammation suggests degeneration in the plantar fascia, and is rarely due to acute trauma.
The pain felt is often sharp, and centered at the inner part of the heel, or the mid-part of the foot. It commonly is worse when getting up in the morning or activity after a long period of sitting. In mild cases, the pain goes away after a few steps, but in more severe cases may worsen as the day goes on.
Plantar fasciitis affects roughly 2 million people in the U.S., and people have a 10 percent lifetime risk of being affected by it.
Causes include overuse, an increase in workout or running activities, being overweight, poor footwear, tight heel cords and hamstrings. Those with abnormalities such as flattened or high arches, and older people are also more prone to it.
 Although many people with plantar fasciitis may also have heel spurs, spurs are not usually the cause of pain. One out of three people has heel spurs, but only one out of 20 people with heel spurs has foot pain. Because the spur is not usually the cause of plantar fasciitis, the pain can be treated without removing the spur.
Although many people with plantar fasciitis may also have heel spurs, spurs are not usually the cause of pain. One out of three people has heel spurs, but only one out of 20 people with heel spurs has foot pain. Because the spur is not usually the cause of plantar fasciitis, the pain can be treated without removing the spur.
Other abnormalities may include inflammation at the back of the heel (insertion of the Achilles’ tendon), loss of the protective fat pad under the heel, or nerve irritation next to the plantar fascia (Baxter’s neuritis).
Plantar Fasciitis Treatment
More than 90 percent of patients with plantar fasciitis will improve without surgery. This may take many months to improve.
- Stretches: Plantar fasciitis is made worse by tight muscles in your feet and calves. Stretching your calves and foot is the best way to relieve the pain that comes with this condition. Stretches should be done four times a day.
- Night splints: Most people sleep with their feet pointed down. This tightens the plantar fascia and is one of the reasons for morning heel pain. A night splint stretches the plantar fascia while you sleep. Although it can be hard to sleep with, a plantar fasciitis night splint works well and does not have to be used once the pain is gone. There are several styles of plantar fasciitis night splints available online.
- Physical therapy: A structured physical therapy program will focus on exercises to stretch the calf muscles and plantar fascia. In addition to stretching as noted above, physical therapy may also involve special treatments to decrease inflammation such as taping, ice treatments, massage, and strengthening muscles that prevent the foot from rolling inwards and protect the plantar fascia.
- Rest: Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to adjust activities where your feet pound on hard surfaces (for example, running or step aerobics). In some cases, your foot could be immobilized in a boot or cast or you may need to be on crutches to take your weight off your foot.
- Non-steroidal anti-inflammatory Drugs (NSAIDS): Medicines such as ibuprofen or naproxen reduce pain and inflammation. They are used during the first part of treatment.
 Heel protection: Shoes with thick soles and extra cushioning can reduce pain with standing and walking. A Visco or Tuli’s heel cup can also be helpful in protecting the heel and easing pain.
Heel protection: Shoes with thick soles and extra cushioning can reduce pain with standing and walking. A Visco or Tuli’s heel cup can also be helpful in protecting the heel and easing pain.- Orthotics: In some cases, prescriptive orthotics are needed to help with structural abnormalities that may cause plantar fasciitis.
- Cortisone injections: Cortisone, a type of steroid, is a powerful anti-inflammatory medication. It can be injected into the plantar fascia to reduce inflammation and pain for temporary relief. However, injections should be limited due to the risk to the soft tissue. Many steroid injections can cause fat pad weakening or the plantar fascia to rupture (tear), which can lead to a flat foot and chronic pain. Injections are used for cases that don’t improve with initial treatment.
Virtual Visits Are Available
Safe and convenient virtual visits by video let you get the care you need via a mobile device, tablet or computer wherever you are. We'll assess your condition and develop a treatment plan right away. To schedule a virtual visit, call 414-777-7700.
More to Explore





