The Froedtert & MCW Blood and Marrow Transplant (BMT) and Cellular Therapy Program offers CAR T-cell therapies and other cellular therapies for patients with certain types of lymphoma, myeloma, leukemia and several other blood cancer types.
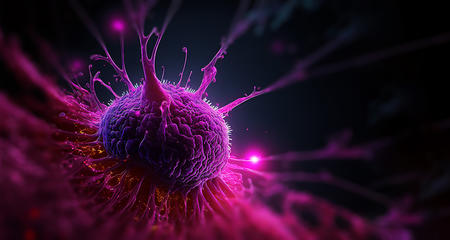
With CAR T-cell therapy, re-engineered T cells are infused back into a patient to become part of the immune system where they can then identify and attack unique cancer cells.
A unique CAR T-cell therapy approach developed by MCW physicians and researchers in a phase I clinical trial used autologous T cells engineered to recognize CD19 and CD20 molecules (also called antigens) on a cancer cell’s surface. Results from this trial (now closed) were published by the researchers, and the trial led to further study in multicenter trials in the U.S. and Europe.
For more information on clinical trials exploring CAR T-cell and other cellular therapies, please talk with your doctor. We post new clinical trials when they are available to eligible patients.
The BMT and Cellular Therapy Program also offers commercially available CAR T-cell products.
- Axicabtagene ciloleucel (YESCARTA®) – For certain patients with B-cell lymphomas; targets the CD19 antigen.
- Tisagenlecleucel (Kymriah®) – For certain patients with acute lymphoblastic leukemia, diffuse large B-cell lymphoma and follicular lymphoma; targets CD19 antigen.
- Lisocabtagene maraleucel (Breynazi®) – For certain patients with large B-cell lymphomas and follicular lymphoma; targets CD19 antigen.
- Idecabtagene vicleucel (Abecma®) – For certain patients with multiple myeloma; targets B-cell maturation antigen (BCMA).
- Ciltacabtagene autoleucel (Carvykti®) – For certain patients with multiple myeloma; targets BCMA.
- Brexucabtagene autoleucel (Tecartus®) – For certain patients with mantle cell lymphoma or acute lymphoblastic leukemia; binds to CD19 antigen and normal B cells.
Who Can Have CAR T-Cell Therapy
Along with FDA-approved commercial products, other forms of CAR T-cell therapy are being studied for their safety and effectiveness through clinical trials. These options are available for eligible patients who have certain types of lymphoma, myeloma, leukemia and several other blood cancer types, when their disease has not responded to other treatment such as chemotherapy and radiation therapy. CAR T-cell therapy may be offered to you after a thorough evaluation of whether or not you may benefit.
Additional CAR T-cell therapies are being explored to treat people who have acute lymphoblastic leukemia.
If CAR T-cell therapy is not for you, be sure to ask your doctor about other clinical trials or treatments that may be best suited for your particular situation. Call 414-805-0505 for information.
How CAR T-Cell Therapy Works

The first step is a complete evaluation of your current health and your cancer treatment history. If your doctor thinks you could benefit from CAR T-cell therapy in a clinical trial with an FDA-approved CAR T-cell therapy or from another type of cellular therapy, you’ll be connected for consultation with a physician specializing in the proposed treatment.
When you have been cleared to participate in CAR T-cell therapy, your care team will guide you through the process of preparing to receive treatment.
- Apheresis — A blood draw, followed by the process of extracting T cells from your blood in a lab.
- Your T cells will be brought to a Medical College of Wisconsin lab on the same campus as Froedtert Hospital for the process of combining the T cells with a receptor called CAR or chimeric antigen receptor. Depending on the type of CAR T-cell product you are receiving, we may send your T cells to an out-of-state lab for similar processing.
- In the labs, the combined cells are grown until there are hundreds of millions of them.
- Lymphodepletion — About a week before treatment, you’ll receive chemotherapy and other drugs to deplete the body of any remaining T cells, preparing you to receive the cancer-fighting CAR T-cell therapy infusion.
- At Froedtert Hospital, you will receive your personalized CAR T-cell therapy via an IV infusion in a single dose. This takes about one hour, but you may need to stay in the hospital for two to seven days. Some CAR T-cell therapies can be given in the outpatient setting rather than during a hospital stay. The CAR T cells multiply in the body and spread to find and attack specific cancer cells. When your doctor feels your condition is stable enough for release, you’ll be discharged home.
CAR T-Cell Outpatient Care
Similar to CAR T-cell therapy delivered during a hospital stay, outpatient CAR T-cell therapy is for people who have certain types of leukemia, lymphoma, multiple myeloma or other conditions and diseases involving immune deficiencies. Outpatient CAR T-cell therapy offers the same benefits as CAR T-cell therapy given during a hospital stay. The difference is that there is no need for hospital admission during the course of outpatient treatment and monitoring. Outpatients have the flexibility to rest and recover after treatment in the comfort of their own home or at a nearby accommodation. This may be a favorable option for some patients, families and caregivers.
Outpatient CAR T-cell therapy is not the right choice for everyone. It is offered on a case-by-case basis after a thorough evaluation by our CAR T-cell therapy team. You may be eligible for CAR T-cell therapy if you meet the following criteria:
- You have been evaluated by a doctor on our CAR T-cell therapy team who deems outpatient therapy appropriate and safe.
- Aside from cancer, you are in good physical condition with no significant medical problems (e.g.,. heart or kidney disease).
- You live within an hour of the Clinical Cancer Center on the Froedtert Hospital campus or are willing to stay at a designated hotel/lodging for the duration of treatment (e.g., Kathy’s House).
- A responsible caregiver can accompany you to all appointments and provide 24/7 care, support and transportation during your treatment.
- You can accommodate daily visits to our BMT/CAR T-cell therapy unit within our Day Hospital as directed.
If you meet the criteria for outpatient CAR T-cell therapy, you can be confident that our specially trained CAR T-cell team will keep you safe by monitoring you very closely for side effects or infections that require hospitalization. We are committed to providing safe, high-quality care regardless of the care setting.
CAR T-cell therapy offered in the outpatient setting involves the same course of treatment (evaluation, conditioning, infusion, engraftment and recovery) as when patients receive it in the hospital.
In the outpatient setting, patients make daily visits to the outpatient BMT/Cellular Therapy unit in the Day Hospital on the third floor of the Clinical Cancer Center on the Froedtert Hospital campus. The outpatient unit is open from 7 a.m. to 8 p.m., Monday through Friday and 7 a.m. to 5:30 p.m. on weekends.
Tests and infusions are performed on the unit in a private treatment room equipped with a comfortable bed and private bathroom. You may read, watch TV or surf the internet during treatment. CAR T-cell therapy is given in a single dose via an IV infusion, which takes about an hour. Daily visits to the Day Hospital continue for two to four weeks, as your doctors will monitor you closely. You will spend two to six hours each day in the unit for two to four weeks.
Risks, Side Effects and After Discharge
You will be carefully monitored for side effects for 28 days after receiving CAR T-cell therapy — while in the hospital and after discharge home.
Side effects can be mild to moderate in severity, but some people experience severe, life-threatening reactions (cytokine release syndrome, neurotoxicity) that require treatment in the hospital. The 28-day monitoring period is designed to make sure there is early intervention for side effects. At the Clinical Cancer Center, physicians and clinical staff have developed and carefully follow guidelines to manage side effects that may occur.
After you have been discharged home, the Froedtert & MCW 24-Hour Cancer Clinic is another resource to help with unexpected, urgent issues that may arise (pain, fever, nausea and other common, cancer-related problems).
Is CAR T-Cell Therapy Effective?
While cellular therapies like CAR T-cell therapy are still relatively new — some are FDA-approved, while others are still investigational — they are developing into promising treatments. Studies show that some patients will see a complete response to treatment (no evidence of disease after CAR T-cell therapy). Physicians and researchers are still studying new ways to engineer cancer-fighting T cells and the most effective way to use them to treat patients and extend life.
Insurance Coverage
Individual insurance coverage will vary. Our financial counselors and navigators will help you determine your coverage and any financial responsibilities you should be prepared for with CAR T-cell therapy.
Nationally Accredited
Our facility has long been accredited by the Foundation for the Accreditation of Cellular Therapy (FACT). In addition, we were one of the first in the nation to receive specific FACT accreditation that enables our physicians to offer treatment with immune effectors like CAR T-cell therapy. (Immune effectors are activated cells — such as T cells — that defend the body in an immune response.)
Internationally Recognized and Experienced in BMT and Other Cellular Therapies
Our physicians are internationally recognized for their research and for treating patients with innovative cellular therapies. They were early pioneers of techniques in stem cell transplantation, immunotherapies and CAR T-cell therapy, helping discover how the body’s own immune system has the power to fight cancer. MCW hematologist/oncologist William Drobyski, MD, was among the first researchers using a donor’s T cells to eradicate cancer after bone marrow transplantation.
More to Explore