Many patients respond well to the use of the various medication options available to relieve the symptoms of movement disorders. Our Parkinson’s and Movement Disorders team is up-to-date in prescribing the latest, most effective medications.
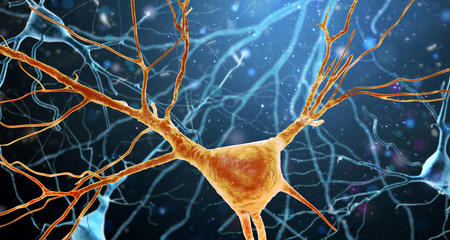
Most symptoms of Parkinson’s disease are caused by a lack of dopamine within the brain. Most Parkinson's disease drugs are targeted at replenishing or mimicking dopamine. These drugs reduce muscle rigidity, reduce tremor, and improve speed and coordination of movement. Medication may be changed or the dose may be adjusted depending on the severity of symptoms. Common groups of drugs used to treat Parkinson’s disease and other movement disorders include levodopa, dopamine agonists, MAO-B antagonists, COMT-inhibitors, anticholinergics, amantadine and antidepressants.
Botulinum Toxin to Treat Muscle Spasms, Voice and Speech Impairments
Botulinum Toxin can be used to treat different movement disorders such as dystonia, hemifacial spasm, blepharospasm, spasticity, and muscle spasms. Froedtert & the Medical College of Wisconsin is highly experienced with this procedure. The approach uses neurotoxins, injected in small amounts, to disrupt the flow of nerve impulses to excessively contracted or spastic muscles, reducing movements for a period of weeks or months.
Four formulations of botulinum toxin are currently approved by the Food and Drug Administration for use in selected medical conditions. These are onabotulinumtoxinA (Botox), incobotulinumtoxinA (Xeomin), abobotulinumtoxinA (Dysport) and rimabotulinumtoxinB (Myobloc).
Collagen injections are used to treat voice and/or speech impairment for patients with Parkinson’s disease.
Contraindicated Drugs for Parkinson's Patients
Several medications should not be taken by Parkinson’s patients because they alter the brain’s dopamine system. Always let your neurologist know before you have surgery, so he or she can work with your medical team to keep your Parkinson’s in control. View a list of drugs that Parkinson’s patients should not take.
Medication Management for Parkinson's Disease (On/Off Testing)
As Parkinson’s disease progresses, some individuals may need to increase the dosage of their medication to control symptoms. With time, patients may notice that, throughout their day, they have periods of good symptom control (“on” time), periods in which symptoms are much more noticeable (“off” time), and even periods in which peak medication levels produce involuntary movements (dyskinesias). When people experience these various states throughout the day, they are said to have motor fluctuations (sudden changes in the ability to move).
When assessing a patient’s response to medication, the Parkinson’s neurologist may ask the patient to come to the clinic “off meds,” usually foregoing their Parkinson medications for 12 to 24 hours. The doctor will then perform the usual exam utilizing the Unified Parkinson Disease Rating Scale (UPDRS), gaining valuable information on the patient’s baseline Parkinson’s disease in the drug-free state.
After this first exam, the neurologist will give a dose of medication (usually carbidopa-levodopa, thus the term “L-DOPA challenge,” but sometimes in combination with other medications), wait 30 to 60 minutes and re-examine the patient. At that point, the doctor may give another dose, followed by re-examination. This cycle repeats until the doctor can determine that the patient is either a “responder” or a “non-responder” to medications. It also allows for monitoring of potential side effects, like nausea, dizziness, low blood pressure, etc.
Furthermore, the doctor can get a feel for what the patient’s “best on” is, meaning how much improvement can be expected with a given dose of medication. This can help guide both medication adjustments as well as whether or not deep brain stimulation surgery might be an option. The end result is that, over the course of a morning or afternoon (usually 2-3 hours), the neurologist is able to gain a better understanding of a patient’s Parkinson’s disease and how to best manage it.
Clinical Trials
In some cases, patients have the opportunity to participate in various clinical trials, including clinical drug research trials, being conducted through the Medical College of Wisconsin to test new medications aimed at controlling movement disorder symptoms. Participation is strictly voluntary.
Virtual Visits Are Available
Safe and convenient virtual visits by video let you get the care you need via a mobile device, tablet or computer wherever you are. We'll assess your condition and develop a treatment plan right away. To schedule a virtual visit, call 414-777-7700.
More to Explore