ECMO: How This Respiratory Machine Can Effectively Treat COVID-19 Patients
Usually for patients with life-threatening, heart-related conditions, ECMO is allowing COVID-19 patients more time for their bodies to fight the virus
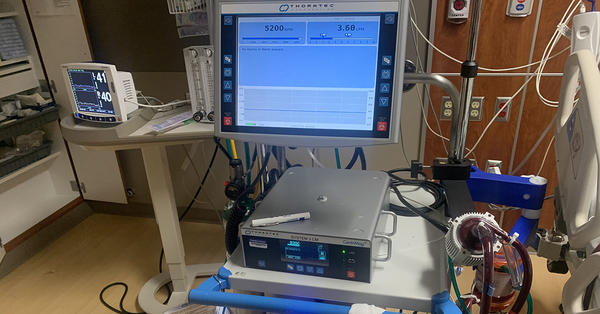
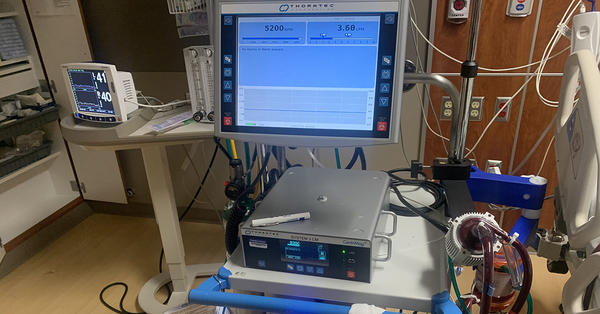
As the world moves forward through this unprecedented pandemic, physicians around the globe are trying to find effective ways to treat and save the lives of COVID-19 patients. One treatment option that is showing promise is the use of extracorporeal membrane oxygenation (ECMO) for COVID-19 patients with severe respiratory distress. By supporting the heart and lungs, the ECMO machine stabilizes patients to allow their body more time to fight the virus. As a Designated Gold Level Center of Excellence by the Extracorporeal Life Support Organization (ELSO), the ECMO team at the Froedtert & the Medical College of Wisconsin health network is uniquely experienced and positioned to help COVID-19 patients.
“We are one of the largest ECMO programs in the Midwest, as we have around-the-clock ECMO-dedicated staff and the capability to run over 16 patients simultaneously,” said Lucian A. Durham, MD, PhD, director of Mechanical Circulatory Support & ECMO at the Froedtert & MCW health network. “ECMO can be a potential game changer for COVID-19, and it’s already proven to be a life saver. Since 2018, more than 200 patients at Froedtert Hospital who’ve been on ECMO longer than 24 hours have recovered.”
How Does ECMO Work?
Originally developed in the 1960s to support newborns and infants with respiratory distress syndrome and cardiac abnormalities, ECMO has only been widely adapted for usage in adults over the last five years. The ECMO machine works by inserting a plastic tube into a large vein and/or artery through the neck, chest or groin of the patient. This tube allows for the patient’s blood to flow out into an oxygenator, or artificial lung. The oxygenator adds oxygen and removes carbon dioxide from the blood, before a pump sends this blood back into the patient through a separate tube, at the same frequency and force of the heart. Essentially, ECMO helps these patients by acting as their heart and lungs.
The machine is used when all other medical options have been exhausted for patients whose lungs can’t provide enough oxygen to their body or rid themselves of carbon dioxide. It can also be used for patients whose heart can’t pump enough blood to the body and for those waiting to either get a heart or lung transplant.
Do I Qualify for ECMO?
Determining when and how long to use ECMO as a treatment for patients is based on several criteria. If you’d like to confirm whether you or a family member meet criteria for ECMO, we recommend you discuss your concerns with your local health care team who can help confirm if ECMO may be appropriate, and inquire about transferring to a local health care center that offers ECMO support.How ECMO Can Help COVID-19 Patients
Even though there’s more to learn about how COVID-19 affects the body, physicians know that it primarily affects the lungs. In certain cases, the virus can entirely overwhelm the lungs and, in turn, negatively affect the heart.
“COVID-19 is different from pneumonia or an influenza A or B because it affects all five lobes of the lung — three on the right and two on the left — and it’s patchy and diffused throughout the whole lung,” Dr. Durham said. “That is where the real respiratory issues come from, as it’s damaging all areas of the lung.”
Because all five lobes of the lung are damaged, they can’t properly exchange oxygen and carbon dioxide. As carbon dioxide levels in the body increase, so does respiratory rate, as the brain tells the body to breathe more to rid itself of this carbon dioxide. However, since the lungs are damaged and are unable to so, this carbon dioxide remains in the blood and turns to acid.
“The body doesn’t work well in an acidic environment,” Dr. Durham said, “particularly, the right side of the heart. The lungs get stiffer and the pressure to push blood through the lungs goes up, known as pulmonary hypertension. This puts strain on the right side of the heart and causes it to fail. When the body fails to this degree, that is when ECMO can help.”
When a COVID-19 patient is transferred to Dr. Durham and the ECMO team, whether by medical intensive care unit physicians within the Froedtert & MCW health network or emergency department physicians from external health systems, a right ventricular support device (RVAD) and oxygenator within the ECMO machine is used. The RVAD is placed inside the patient through the tube that goes into the patient’s neck, down through the right atrium and right ventricle of the heart and into the pulmonary artery. This allows for blood to be taken out of the right atrium and sent to the ECMO machine. There, it’s filtered, temperature-modulated and oxygenated, and the carbon dioxide is removed. This blood then enters the body through a tube placed into the pulmonary artery.
“We are putting 100% oxygen into those pulmonary arteries, which is what is going out into the two lungs,” Dr. Durham said. “This accomplishes two things: One, it takes the load off the right side of the heart, as we are essentially bypassing it. And two, by increasing the level of oxygen going into the lungs, it decreases pulmonary vascular resistance and reduces the pressure it takes to push blood through the lungs.”
This ECMO process supports patients’ bodies and allows them extra time to attack and overcome the virus. This extra time that they are allotted is often necessary for patients in such extremes, with the average COVID-19 patient staying on ECMO for 35 days. Once off ECMO, they then remain isolated while recovering in the cardiovascular intensive care unit.
An Added Layer of Safety for COVID-19 Patients on ECMO
Certain patients with an aggressive form of COVID-19 are susceptible to a “cytokine storm,” which can cause a severe inflammatory response and multiple organ failure. This happens when a patient’s immune system malfunctions and attacks its own cells. While ECMO alone has been shown to reduce the chances of a cytokine storm, the Froedtert & MCW health network is the first institution in Wisconsin to utilize CytoSorb Filter, a device that is used within ECMO to further reduce the cytokines and inflammatory molecules.
Recently approved by the Food and Drug Administration for temporary emergency use in COVID-19 patients, CytoSorb is a sterile, single-use filter that is placed into a patient’s ECMO circuit. This filter contains absorbent polymer beads that are designed to remove cytokines — what signals the immune system to work against itself — as blood passes through. This filter is then replaced routinely for a five-day course of treatment.
Advancing COVID-19 Care with ECMOCARD Observational Study
With one of the largest ECMO programs in the Midwest, the Froedtert & MCW health network is one of 239 health centers on six continents — and the only in Wisconsin — that is participating in the Extracorporeal Membrane Oxygenation for 2019 Novel Coronavirus Acute Respiratory Disease (ECMOCARD) observational study to advance COVID-19 treatment. Each participant is sending data and information to the University of Oxford in England on how their health center is using ECMO for COVID-19 patients. At Oxford, artificial intelligence and neural networking will be analyzing the data and information in hopes to find exactly what type of ECMO treatment or combination of ECMO treatments are best for COVID-19 patients.
“This is one of the largest multicenter, multinational observational studies that’s ever been done,” Dr. Durham said. “Many of the hospitals have different ways of treating these patients. The data on how they’re treating them and what their outcomes have been from a pulmonary, cardiac and neurologic standpoint will help shape the way care is delivered in the future from an ECMO standpoint.”
The Earlier, the Better for ECMO
Although ECMO has already shown to be a promising way to save lives, Dr. Durham urges medical professionals to get patients to ECMO teams earlier, as this could save even more. Getting certain patients on ECMO sooner rather than later can avoid organ failure that physicians are seeing with COVID-19.
“The patients we get earlier are the ones we have the greatest impact on,” Dr. Durham said.
Learn more about the advanced cardiac procedures the Froedtert & MCW team offers.
If you’re a physician looking for more information about our ECMO Program, call 414-805-4700.



Interested in ECMO.
Hi Lisa - ECMO is one of the advanced treatment options available to treat critically ill patients who are in lung or heart distress, including those in cardiogenic shock. For more information, please visit https://www.froedtert.com/cardiogenic-shock. Thanks, Claire
Is this ECMO available in NY state?
Hi Annette – ECMO is available at select locations across the country. Please contact your local health care provider for information on its availability in your area. It’s important to note that a patient cannot opt to undergo treatment via ECMO. This treatment is available for critically ill patients. Thanks, Claire
Thank you.
....has it occurred to anyone that extracorporeal membrane oxygenation might work even better if you add O3 (ozone)? see, for example,
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7733684/
and especially
https://clinmedjournals.org/articles/jide/journal-of-infectious-disease…
Ozone therapy has been around for a long time. From what I've read,
I'd recommend it as a tier-1 (immediate) antiviral treatment. ECMO is a stone's-throw away from DIV. I'd like to know why the medical community isn't using this as it appears it would benefit COVID infected patients immediately, is extremely cost-effective and is available ad hoc,
as opposed to the current dearth of vaccines from Pfizer et al......
If while in care a patients lungs white out while intubated and their blood oxygen saturation has dropped to 70 is that a good time to have them be put on ECMO?
Hi Jordan - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Is this an effective treatment if deemed necessary for a patient that is also in treatment for T-cell Lymphoma, that has gotten the virus?
Hi Robert - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
If someone has been intubated for 10 days and lungs are starting to show scarring, would ECMO be an option?
Hi Victoria - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Please respond ASAP. I need to know the criteria
Hi Sarah - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
What is the criteria for receiving ECMO? Is there a point where it is "too late" to receive ECMO after being on ventilator?
Hi Amanda - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Will this work for a patient that has been ventilated for a few days whose oxygen is maintaining in the mid 90’s only when on their stomach?
Hi Megan - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
How can this be used at a hospital that doesn’t have one? We hope that somehow this can be brought to a specific hospital, as we are worried of moving the patient to another hospital.
Thank you for your inquiry. Our team works with hospitals across the region to safely transport patients in need of advanced care. Pending your location, your local hospital could connect with our team about a patient transfer.
What is the criteria for receiving ECMO? Is there a point where it is "too late" to receive ECMO after being on ventilator? This should only be received once the patient goes in to ventilator or we can start using while patient is on HFNO?
Hi Neha - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
could you please send the same mail to me
Hi Nayan - We have followed up with you via e-mail with more information.
What is the criteria for receiving ECMO? Need information asap if this is an option.
Hi Kristi - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Can you please send me the ECMO criteria? Need information asap.
Hi Megha - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
There lies the future
Can you send me ecmo criteria?
Hi Shivangi - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Could you send me the criteria for receiving ECMO for covid?
Hi Dawn - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Please can you forward me the criteria for ECMO
Hi Smitha- Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Can you please send me the criteria for ecmo.
Hi Kathleen - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Can you please send me the criteria ECMO.
Hi Mary - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
Please send the info to me I have a friend that is deathly sick with covid thank you
Hi Sandra - Determining eligibility and timing for ECMO is based on several criteria that can vary for each patient. We recommend that you connect with your friend's local health care team to determine if ECMO is an appropriate treatment based on your friend's condition.
By when is a covid patient not a candidate for an ECMO
Hi Guadalupe - Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
What's the criteria for the ECMO? Thank you
Hi Tawana- Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
my dad has severe covid pneumonia, can you please let me know what the criteria is for ECMO treatment?
Hi Kelly- Determining the need for ECMO is based on several criteria. We have followed up with you via e-mail with more information.
There is an 52 y/o Army veteran fighting for her life, as most Covid patients who fall ill do. What is the criteria for receiving ECMO? Is there a point where it is "too late" to receive ECMO after being on ventilator? Where are the facilities who have ECMO? Is this facility an option for transfer. Please advise as time is running out quickly. Thank you.
Hi Jeanette - Thank you for your inquiry. Determining when to use ECMO is based on several criteria. We would recommend that the patient's family discuss these concerns with her medical team and inquire about transferring to a local health care center that offers ECMO support.
Our friend who entered the hospital back in November was at a small hospital with no ecmo. His oxygen level was 30% when he went in. They put him on a ventilator but after a day or two they had it turned to 100% with no progress. His wife gave per for them to transfer him to a larger hospital that had an ecmo. The doctors weren't even sure if that would save him but eventually it did. He was in tbe hospital then rehab for a total of 6 months. He had multiple infections, blood pressure problems, his heart stopped and they did CPR, he got fungal pneumonia, and on and on. But, the ecmo was the one thing that saved his life.