When medication stopped working, our team suggested deep brain stimulation (DBS) to treat Gerry Zylka's Parkinson's disease. See the remarkable results.
We offer deep brain stimulation (DBS) surgery as an option for patients with Parkinson's disease and other movement disorders such as tremor and dystonia. It is also used to treat some epilepsy patients.
DBS is a complicated procedure that requires a skilled and knowledgeable surgical team and highly specialized equipment.
What Is Deep Brain Stimulation?
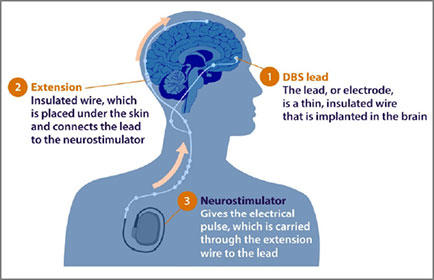
DBS involves brain surgery to place one or more electrodes in the brain. An extension connects the leads to a battery-operated device called a neurostimulator. The neurostimulator is like a heart pacemaker, but for the brain. It is implanted in the patient's upper chest.
Once the neurologist programs the neurostimulator, it delivers small amounts of stimulation to the brain to help control abnormal brain activity. The amount of stimulation can be controlled and adjusted to manage the symptoms of Parkinson's disease, essential tremor and dystonia that do not improve with medications. Some symptoms may not improve with DBS.
DBS is an effective treatment for many patients, but it only treats the symptoms of the disease, not the disease itself. It is not a cure and does not stop the disease progression. DBS can improve such symptoms as:
- Tremor (shaking)
- Slowed movements (bradykinesia)
- Stiffness (rigidity)
How DBS Works
Used with permission from parkinsonsdisease.net.
DBS involves implanting a thin wire, or lead, containing one or more electrodes, in the brain. The lead extends through a small opening in the skull and connects to a neurostimulator — a device that is similar to a heart pacemaker, only for the brain. The surgeon then implants the battery-operated neurostimulator under the skin in your upper chest.
After programming, the neurostimulator delivers controlled and adjustable levels of electrical signals to the brain to soothe symptoms of Parkinson’s disease, tremor and dystonia that fail to improve with medications.
Candidates for Deep Brain Stimulation
The Parkinson’s and Movement Disorders team meets weekly to review patient cases, including patients who may be candidates for the deep brain stimulation procedure. Patient selection is based on a thorough analysis of their medical situation and needs, as well as the best evidence available in medical literature and our extensive experience in performing DBS procedures.
Possible candidates for DBS include:
- Patients who have symptoms for at least 3 – 4 years.
- Patients with Parkinson's disease, essential tremor and dystonia who experience movement-related symptoms that cannot be controlled by medications or experience side effects from those medications
- Patients who show no significant problems with thinking and memory
New uses for DBS are being investigated, including symptom control for patients with epilepsy, Tourette’s syndrome, depression and chronic pain syndromes.
DBS has been successful in treating patients as young as 13 years old. In general, surgery is performed on patients under 75 years old, but this is not a firm guideline. Each patient must be assessed individually in regard to his or her stamina and overall health.
Thanks to significant innovation in DBS therapy, we offer three FDA-approved DBS devices. You and your movement disorder neurologist will thoroughly discuss the differences between the three options and determine which one meets your needs.
When to Consider DBS
There is a window of opportunity when DBS is an effective treatment, typically in the eight to 12-year range. If you wait beyond the window, symptoms may be too severe to respond.
- For essential tremor and dystonia, DBS should be considered after symptoms have failed to improve with one or more medications and the tremor interferes with daily activities.
- For Parkinson's disease, DBS should be considered if you've had symptoms for at least four years and your symptoms still respond to carbidopa-levodopa, but the medication causes significant fluctuations or side effects (wearing off, dyskinesias, freezing, dystonia).
If you qualify for DBS, you make a commitment to the process since the workup for DBS and the procedure requires several visits to the clinic and hospital. It is important to determine on medical and personal levels if DBS is right for you.
The screening and evaluation process includes multiple steps.
- Consultation where we take a complete medical history and perform a neurological exam
- Videotaped off-on testing where your motor symptoms are rated after you are off medication for 12 hours, then medication is taken and you are monitored while you are on medication
- Neuropsychological testing that assesses thinking skills, motor, behavioral, language and executive function (Make sure you bring any glasses or hearing aids, as well as a friend or family member.)
- DBS Case Conference with the Movement Disorders team to determine if you are a good candidate.
If you are a good candidate, you will be referred to a neurosurgeon and team to develop a procedure plan.
What to Expect During DBS Surgery and How to Prepare
Before surgery, you can expect the following - dependent on your individual situation. The team will help you scheduled appointments and determine which steps are necessary. Bring a list of your current medications to all of your appointments.
- Presurgical MRI for planning purposes is done with oral sedation or general anesthesia, if needed.
- Preadmission testing includes a physical exam for medical clearance and a discussion of all of your medications and supplements.
- Antibacterial skin treatment 2 to 5 days before surgery, if indicated.
Computerized brain-mapping technology helps the surgeon find the precise location in the brain that generates the nerve signals that cause tremors and other symptoms. Imaging and recording equipment map both the physical structure and brain function.
You will be asked to hold or stop all medications you take for tremor or dystonia control the morning of the procedure. This helps the success of the procedure.
DBS Lead Placement

In the preprocedure area, your head will be shaved completely and a frame applied. The frame is used to keep the head completely still and to help with locating the specific target areas in the brain. For your comfort, local anesthesia will temporarily numb the areas where the frame is attached. Once the frame is placed, you will have a CT scan of your head on the way to the procedure room.
To allow the surgical team to assess brain functions, most patients need to be awake during surgery. A local anesthetic numbs the scalp while the surgeon makes the small opening (about the size of a dime) in the skull. Due to the unique nature of the human brain and its inability to generate pain signals, patients experience no pain while we place the electrodes in the brain. Be sure to tell your provider if you are experiencing any discomfort along the way. Asleep DBS surgery is an option, but is only offered on a specific case-by-case basis.
During the procedure, you will be able to move your arms and legs, and talk to the team. Your team will request your participation with questions and evaluate your tremor to make sure they have located the correct placement.
Another CT scan will be done after the procedure. You will recover for 1 to 2 hours in the postprocedure recovery area and transfer to the neurosciences specialty unit. The DBS team will give your family an update.
Following the lead (electrode) procedure, you will stay overnight in the hospital for observation. Your incision will be closed with a surgical glue that dissolves over 2 to 3 weeks. The night of the procedure you should be able to eat dinner and get out of bed to walk around your room. We will go over wound care, bathing and activity instructions before you leave the hospital. You may notice immediate improvement of your symptoms, but it is important to continue all medication as prescribed by your doctor.
DBS Neurostimulator Placement
The final stage of the DBS procedure is implanting the neurostimulator about one week after the lead (electrode) is implanted. This is done under general anesthesia, which means you will be sedated (asleep) for the entire procedure.
You should plan to take all tremor or dystonia related medications the morning of your neurostimulator implant procedure. Since you will be asleep for this procedure you will not need to hold these specific medications.
This is an outpatient procedure and you should expect to be discharged from the hospital that day procedure. Your incision will be closed with glue for this procedure as well.
All of the DBS hardware is internal (inside the body). Nothing is outside of the skin. The neurostimulator (battery) will not be turned on following the procedure because the site needs time to heal. You may experience mild swelling, pain and bruising at the implant site.
DBS Device Programming
The neurostimulator is usually turned on and programmed 3 to 4 weeks after the electrodes are placed. The initial programming takes place during an extended clinic visit with your neurologist and the DBS nurse. A wound check is also done at this time.
You will be asked to follow some special instructions so we can see how the medications and the stimulation work together. The neurologist and/or the DBS nurse will use a handheld device called a programmer to adjust the settings of the DBS system. During this process, you will be examined and questioned about how and what you may be feeling. The neurologist and/or the DBS nurse will be looking for improvement in your:
- Tremor
- Rigidity
- Bradykinesia
- Dyskinesia
They will also be watching for side effects such as:
- Numbness
- Tingling, muscle cramping or pulling
- Abnormal sensations
- Changes in your speech or vision
We will teach you how to use your own DBS programmer. This device will allow you to check the neurostimulator status, monitor battery life, turn therapy on or off and change some of the settings if needed. Symptoms usually improve right away for tremor, but may take more time for dystonia.
Medications are often adjusted during this time. Patience is critical during the first three to six months after programming starts. It can take anywhere from 3 to 12 months to optimize your DBS settings and medications.
Care After DBS Surgery
Over the next weeks or months after we activate the neurostimulator, we will make a series of adjustments in the electrical pulse. For the initial follow up visits and stimulation adjustments, you will need to travel to the same location as the surgery. After that, electrical programming can take place at any medical facility that has a specialist with the expertise and equipment.
One DBS device was recently approved for remote programming by the U.S. Food and Drug Administration for patients with essential tremor and Parkinson’s disease. This allows you to interact virtually with your neurologist and ensures the ability to optimize DBS settings and functionality. It reduces the need for in-person appointments for adjustments — eliminating drive time and time off from work. We are excited to be the first in the state of Wisconsin to offer this opportunity to patients with this particular DBS device.
DBS Surgery Risks
As with any surgery, the procedure is not risk free. There is about a 1 to 3% chance of brain hemorrhage that may be of no significance or may cause paralysis, stroke, speech impairment or other major problems. This means that for every 100 patients who undergo surgery, one to three will experience a permanent or severe complication. However, this also means that most patients will have no serious complications.
There is a 15% chance of a minor or temporary problem that resolves quickly or over a short period of time. Rarely, infections occur. While treatment of infection may require removal of the electrode, the infections themselves have not caused lasting damage, and we can implant the device again after the infection clears.
The electrode that is implanted in the brain and the electrical systems that provide stimulation are generally very well accepted by the brain with no significant changes in brain tissue around the electrodes. The neurostimulators implanted in the chest that produce the stimulation have a limited life span and will require future surgery to replace them.
Avoiding Complications
Any procedure has risks, one is the possibility of infection or a non-healing surgical wound. These can be avoided by following these instructions.
- Remove the dressing(s) on day #3 after surgery.
- Keep incisions clean and dry.
- Wash hands often.
- Watch for signs and symptoms of infection.
- Do not scratch or pick at incisions.
- Do not use lotions, creams or powders on incision sites.
- Do not lift more than 10 pounds.
- Do not submerge the incisions.
Please contact your doctor's office if you experience any of the following signs or symptoms of infection. In the event of an infection, the device may need to be removed and then replaced once the infection is gone.
- Fever greater than 101 degrees
- Redness, swelling or pain at the incision site
- Drainage around or under the incision
DBS Side Effects
There are some possible side effects with brain surgery and stimulation therapy. Some of the side effects are temporary and can be adjusted by changing the DBS settings. Your health care team will discuss these with you during your consultation.
- Numbness or tingling sensations
- Muscle tightness in face or arms
- Speech or swallowing problems
- Dizziness or lightheadedness
- Balance problems
- Visual disturbances
- Weight gain
- Poor control of symptoms
- Device malfunction
Effectiveness of DBS
While results vary from patient to patient, DBS is remarkably safe and effective in properly selected patients. The beneficial effects of symptom control have been demonstrated to last for several years.
- Most patients with essential tremor may experience an 70 to 80% reduction in their tremors. Some patients may experience 100% reduction of their tremor initially.
- Patients with Parkinson's disease who have initially responded well to medications but over time have developed side effects can experience significant improvement in motor symptoms (such as tremor and slowness of movement) and potentially reduce medications by 50% which reduces medication related involuntary movements (dyskinesias).
- DBS can increase the amount of “on-time for people with Parkinson's disease by 4 to 6 hours per day.
- Dystonia patients benefit from a reduction of involuntary muscle contractions, and shaking subsides for patients with essential tremor.
- People with epilepsy who undergo DBS may have fewer seizures.
- Most patients are able to significantly reduce their medications following deep brain stimulation.
Frequently Asked Questions
-
Is DBS covered by insurance?
Medicare and most private insurance companies will cover most, if not all, of the costs. Our Neurosurgery Clinic team will work with your insurance company to determine the coverage. You may be responsible for deductible or copay amounts.
-
Can I stop my medications after the DBS procedure?
For essential tremor/dystonia, this depends on the individual. Oftentimes patients with ET are no longer on meds because they were not effective.
-
Can people see my battery?
There will be scars where the incisions were made. For some, batteries will be more noticeable, like a lump under the skin, depending on your body build.
-
Can the batteries be recharged?
There are both non-rechargeable and rechargeable devices available. These options will be discussed with you prior to your procedure(s).
-
How often does the battery need to be replaced?
Non-rechargeable batteries have an average life span of 3 to 5 years. Much of this depends on your stimulator settings. Current rechargeable devices have a life span of 9 to 15 years. Some devices will no longer charge if they have depleted completely so it is very important to charge the battery as recommended.
-
Are there any limitations to what I can or cannot do?
Most people can return to regular activity and low-impact exercise two weeks after the DBS procedure. Specific instructions will be provided following your procedure.. You should plan to avoid massage, neck manipulation and other activities that come in direct contact with the device.
-
Can I travel a DBS device?
Yes, you can travel with DBS system implanted. There are no travel restrictions. You may set off a metal detector at the airport, so please discuss this with the care team during your consultation.
-
Do I need to take antibiotics before having dental work after the DBS is implanted?
You do not need to take antibiotics for routine dental visits and cleanings. For invasive dental procedures, it is recommended that you take oral antibiotics. Speak with your doctor if you need to have an invasive dental procedure.
-
How long will I need to take off work?
This will be different for everyone. You can expect to take some time off for the procedures, recovery and appointments. Speak with your doctor to determine a plan that is best for you.
-
How long will I be restricted from driving?
We recommend no driving for two weeks following a procedure or if you are taking any narcotic (opioid) pain medications.
Virtual Visits Are Available
Safe and convenient virtual visits by video let you get the care you need via a mobile device, tablet or computer wherever you are. We'll assess your condition and develop a treatment plan right away. To schedule a virtual visit, call 414-777-7700.
More to Explore