Robotic prostatectomy using the da Vinci® robotic surgical system is a minimally invasive procedure for prostate removal.
A robotic prostatectomy is performed laparoscopically through a series of small incisions, instead of the one four-incision needed for an open prostatectomy. The small incisions result in a shorter post-operative recovery and a faster return to normal activities. There is also less scarring and blood loss than in an open prostatectomy.
Available data suggests potency and continence rates are similar between the two approaches. Longer follow-up with robotic prostatectomy will be needed to determine if cancer control rates are the same as those achieved by open surgery.
Precision Surgery
The system’s magnification and 3-D visualization work together to enhance the surgeon’s viewing of the prostate, nerves, bladder and surrounding structures. It offers the surgeon the same dexterity as the human hand by “translating” the surgeon’s hand movements into the precise movements of the robot’s micro-instruments. This allows the surgeon to remove the prostate and nearby areas of concern, while sparing structures that may negatively impact urinary control and sexual function.
What to Expect
During the robotic procedure, a patient is placed under general anesthesia and positioned on his back. The surgeon makes six small incisions in the patient’s abdomen.
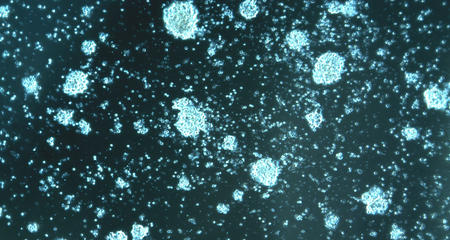
Hollow cylinders called ports are placed in the incisions, and an operating telescope, camera and surgical instruments are inserted through the ports and into the abdomen. The robot is then positioned at the operating table, and the robotic arms and camera are connected to some of the ports. The surgeon sits at a console a few feet away from the patient, controlling the robotic arms and camera. The surgeon views the surgical area through 3-D goggles, which provide fine details of the body structures.
Once the prostate has been detached from surrounding structures and the urethra (urine tube) has been reattached to the bladder, the robotic arms are removed from the patient. The incision near the navel is enlarged so the entire prostate gland can be removed at once. This is important so that a pathologist can accurately determine the stage of the cancer. All of the instruments are removed, and a temporary urinary catheter and abdominal drain are left in place before the patient is awakened from anesthesia.
While all precautions are taken to reduce the likelihood of complications, no surgical treatment is completely without risk. Potential complications include infection, bleeding requiring blood transfusion, urinary incontinence, erectile dysfunction, port-site hernia and injury to adjacent organs.
After surgery, patients usually spend one or two days in the hospital. During the first day, the patient recovers from anesthesia and receives intravenous (IV) pain medication. By the next day, oral pain medication is usually sufficient. Once pain is under control and bowel function begins to return, patients are ready for discharge.
Post-Operative Care
Patients are discharged home with the urinary catheter, which usually remains in place for about one week. During this time, patients are encouraged to walk often. They may shower, but should avoid swimming or sitting in a bathtub.
Patients then return to the Urology Clinic at Froedtert & the Medical College of Wisconsin for a cystogram (an X-ray of the bladder) to ensure adequate healing has occurred and the catheter can be removed.
Urinary control returns after varying lengths of time. Patients are encouraged to wear an absorbent pad initially while they work to retrain the muscles involved in urinary control. Kegel exercises, which strengthen the muscles supporting the urethra, bladder and rectum, are quite helpful. Heavy lifting should be avoided for about four weeks to avoid the formation of hernias at the incision sites.
Follow-Up Care
At the time of the catheter removal, the pathology report concerning the stage of the cancer is shared with the patient. While follow-up treatment will be based on report results, most patients only need to have their PSA level checked on a regular basis. The first follow-up PSA should be checked three months after surgery and then every six months for the immediate future.
More to Explore