Anal cancer is considered rare. It is not as common as colorectal cancer. It affects about 1 in 500 people (compared to about 1 in 22 for colorectal cancer). Anal cancer happens more in people ages 55 and older, and the incidence of anal cancer is higher in white women and Black men.
What is anal cancer?
Anal cancer develops when cancer cells form in the tissues of the anus or anal canal (the tube at the end of the rectum) and start growing and dividing in an uncontrolled way. Anal cancer starts in cells near or just inside of the anus. You can also develop pre-cancerous cells that have a high chance of eventually turning into cancer. Anal cancers don’t usually spread to other parts of the body but when they do spread (metastasize), treatment is more challenging. That makes early detection especially important.
The Difference Between Anal Cancer and Rectal Cancer
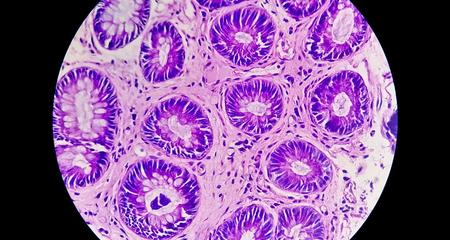
Most anal cancers are squamous cell cancers, meaning they affect the skin-like cells of the anus. In contrast, rectal cancers are different — they develop from the glandular cells - cells produce fluids - in the rectum. (Cancer that starts in fluid producing cells is also called adenocarcinoma.)
While nearly 90% of anal cancers are related to the human papilloma virus (HPV), rectal cancer is not. Treatment is different, too. Anal cancer that hasn’t spread beyond the regional lymph nodes can be cured with chemo and radiation therapy alone, and patients need surgery only if these two treatments don’t completely eliminate the cancer. Early rectal cancer may be treated with surgery alone.
If the rectal cancer has broken through the rectal wall or spread to lymph nodes around the rectum, patients often have radiation and chemotherapy before surgery. Most patients with rectal cancer will not need a permanent colostomy (bag worn outside the body to collect waste), but many will have a temporary ostomy bag.
Symptoms are similar but rectal cancer symptoms also include weight loss for no known reason, anemia, frequent gas, bloating, fullness or cramps.
How do you tell the difference?
If you have a rectal cancer that is very close to your anus, telling the difference between an anal cancer and a rectal cancer may not be possible without a biopsy.
Anal Cancer Symptoms
Around 20% of people who have anal cancer don’t have any symptoms. Some of the symptoms of anal cancer are related to other conditions like hemorrhoids. But if you notice these symptoms, it is important to make an appointment with your doctor.
- Anal itching that doesn’t go away
- A lump or growth in the opening to the anus
- Change in your bowel habits like narrowing stools, more or fewer bowel movements or straining that is unusual for you
- Pain in or around the anal area
- Anal mucus, pus or discharge
- Bleeding from the rectum or anal area
- Swollen lymph nodes (groin, anus)
Causes of Anal Cancer
HPV is linked to more than 90% of squamous cell anal cancers, which are the most common type. It’s important to know that most people who have HPV do not develop anal cancer. As well, some people with anal cancers don’t have any risk factors, and the cause of their cancer is not known. Many studies note that people who smoke have an increased rate of anal cancer. Patients with human immune deficiency (HIV) are also at an increased risk. Anal cancer is not hereditary.
Risk Factors for Anal Cancer
Having HPV is the most common risk factor for anal cancer in men and women. Other risk factors include:
- Other sexually transmitted diseases
- Having more than one sexual partner
- Having anal receptive sex
- Chronic inflammation like anal fistulas
- Smoking
- Having other HPV-related cancers like cervical cancer
- Weakened immune system (such as from HIV or from having an organ transplant)
- Having had pelvic radiation therapy for cancers of the prostate, bladder, cervix or rectum
How You Can Reduce Your Risk or Prevent Anal Cancer
Since anal cancer is caused by HPV more than 90% of the time, consider getting the HPV vaccine. It is also important to practice safe sex — always use a condom. If you are immunocompromised, such as being HIV-positive, make sure to maintain and comply with your treatment. If you smoke, quit. Your primary care doctor can help you with this process.
If you’re at high risk of developing anal cancer, talk with your doctor about a risk reduction and prevention plan, which may include anal cancer screening, especially if you are HIV-positive or HPV-positive. Our high-risk anal cancer screening clinic provides anal cancer screening and monitoring to high-risk individuals, so if anal cancer develops, it can be found early and treated appropriately.
Types of Anal Cancer
There are a variety of anal cancers, but the most common are squamous cell cancers that develop in the skin cells at the anus. Rare types include:
- Adenocarcinomas: Start in cells in the upper part of the anus close to the rectum or in sweat glands in the skin around the anus
- Basal cell carcinomas: A type of skin cancer that develops in the skin around the anus
- Melanoma: Starts in cells in the skin or in the anal lining. These cells produce melanin, which makes the skin brown or black.
- Gastrointestinal stromal tumors: Cancer that usually starts in the cells lining the digestive tract. They rarely start in the anal area.
Diagnosing Anal Cancer
Tests used to diagnose anal cancer include a rectal exam, anoscopy (exam that looks inside your anus with a special scope), and imaging with a CT scan, an MRI and often, a PET scan.
An accurate diagnosis from the start is essential in choosing the best treatment options for anal cancer. The type of anal cancer, its size and the exact location of the tumor affect what treatments will be the most effective.
If you’re at increased risk, talk with your doctor about getting an anal cancer screening, which involves a swab of the anal lining. If something concerning is found with screening, most anal cancers will be diagnosed by having a tissue biopsy taken. This is usually done with local anesthesia in the office or in an endoscopy suite if the tumor is found during a colonoscopy or flexible sigmoidoscopy. In certain cases, taking a biopsy may require the operating room and general anesthesia. This might be needed if it would be very uncomfortable or painful to reach the area to be biopsied.
Anal Cancer Treatment
Treatment for anal cancer needs close coordination within your cancer team, which should include a medical oncologist, a radiation oncologist, and a colorectal surgeon, as well as the expertise of skilled radiologists and pathologists who are familiar with anal cancers. This team effort is important to helping you achieve your best possible outcome.
Treatment will almost always involve a course of concurrent chemoradiation, which means having chemotherapy and radiation therapy at the same time. The areas targeted include the anal tumor and any areas it extends to, as well as lymph nodes in the pelvis and groin. Treatment is daily (Monday through Friday) and lasts about six weeks. Most patients will have a complete response to these treatments. With a complete response — no further evidence of cancer — surgery is not needed.
Even if you haven’t had surgery, a colorectal surgeon is an important member of your team. The colorectal surgeon will see you about eight to 12 weeks after you are done with treatment to monitor your condition. The surgeon will perform an endoscopy to make sure the tumor has gone away. This is done in a clinic visit. If there is still tumor tissue seen at this visit, you will have another check-up in two to three months to give the tumor more time to go away. It is important to know that after chemoradiation, it can take months for the tumor to disappear.
After six months, if the tumor has not gone away completely, your cancer team may recommend surgery or more radiation therapy. This would be recommended if your cancer has spread to nearby lymph nodes or is still in the area where it started.
When anal cancer has metastasized (spread) it often spreads to the liver. It can also spread to the lungs, the bones and distant lymph nodes. For metastatic anal cancer, the goal of treatment with chemotherapy (and sometimes radiation therapy), isn’t to cure the cancer but to control it as long as possible and relieve symptoms.
If anal cancer comes back after treatment, it can return in or around the same place as the original cancer or it may have spread to the liver, lungs or other organs. The treatment goal is to control the cancer and its symptoms. Treatment could involve chemotherapy, surgery, radiation therapy or a combination of these. A clinical trial may be another option. Ask your doctor about a clinical trial for advanced stage or metastatic anal cancer.
Support and Coping With an Anal Cancer Diagnosis
Be sure to stay in touch with your cancer care team, touching base whenever needed about treatment side effects, pain and other circumstances that are concerning to you. Your doctors will see you often throughout your treatment to address treatment side effects. After you are done with treatment, you will have periodic follow-up visits. We are here to support you, answer your questions and direct you to support resources available through our Cancer Network, including emotional support, our 24-Hour Cancer Clinic for pain, nausea and other symptoms that happen outside of usual office hours, financial navigation and financial counseling.
Are there lifestyle changes that are recommended to support side effects of anal cancer treatments? During chemoradiation, your cancer team will give you directions about diet, hydration, skin care and activity levels that are best to help you throughout your treatment.
Questions You Can Ask About Anal Cancer
Your cancer team will spend a lot of time with you explaining your treatment plan, as well as treatment side effects and risks you might experience and how to manage these issues. If you have any questions about your treatment, you will have many chances to meet with your team to get answers to your questions.
Questions Your Doctor Might Ask You
Your doctors will do a thorough medical history and physical exam when they meet you and rule out any conditions or situations that would change the plan to treat you with chemotherapy and radiation, as well as any increased side effects that you could be more likely to have than the average person.
Choosing the Froedtert & MCW Cancer Network for Anal Cancer Treatment
Our doctors specialize in taking care of patients with anal cancer and bring you the most comprehensive and personalized care to treat this cancer. Our high treatment volumes, advanced imaging and precision radiation therapy technologies as well as our highly specialized multidisciplinary care team make this a center of choice for anal cancer treatment.
We have a very specialized and experienced team of doctors and clinicians who have treated a high volume of patients with anal cancer and are ready to take care of you. It begins with being on the leading edge of diagnosing anal cancer in its earliest stages through our High Risk Anal Cancer Screening Clinic, which monitors patients who are at high risk of developing anal cancer due to their risk factors.
The Froedtert & MCW health network is one of the only health systems in the state for evaluating abnormal anal pap smears with high-resolution endoscopy. And, high-resolution endoscopy may also be recommended for people who have had an anal cancer diagnosis in the past, even if they’re not immune-compromised.
Once you are diagnosed, your radiation team will make a plan to deliver very precise, image-guided radiation that is needed to cure anal cancer, even when the cancer is locally advanced. Intensity modulated radiation therapy (IMRT) is an advanced method that can deliver higher doses of radiation more precisely to the tumor while avoiding surrounding tissue. Targeting the radiation precisely to the tumor helps prevent side effects and maximize elimination of the tumor. IMRT can mean fewer side effects from radiation therapy and better quality of life.
Patients with early, as well as locally advanced and metastatic anal cancer, will benefit from the expertise of our colorectal surgeons and our medical oncology team, which has access to the latest drug therapies for treating anal cancer.
Virtual Visits Are Available
Safe and convenient virtual visits by video let you get the care you need via a mobile device, tablet or computer wherever you are. We’ll gather your medical records for you and get our experts’ input so we can offer treatment options without an in-person visit. To schedule a virtual visit, call 1-866-680-0505.
Recognized as High Performing by U.S. News & World Report
Froedtert Hospital is recognized by U.S. News & World Report as high performing in three adult specialties and 16 procedures and conditions, including cancer, colon cancer surgery and gastroenterology and GI surgery.More to Explore